Time Series Analysis
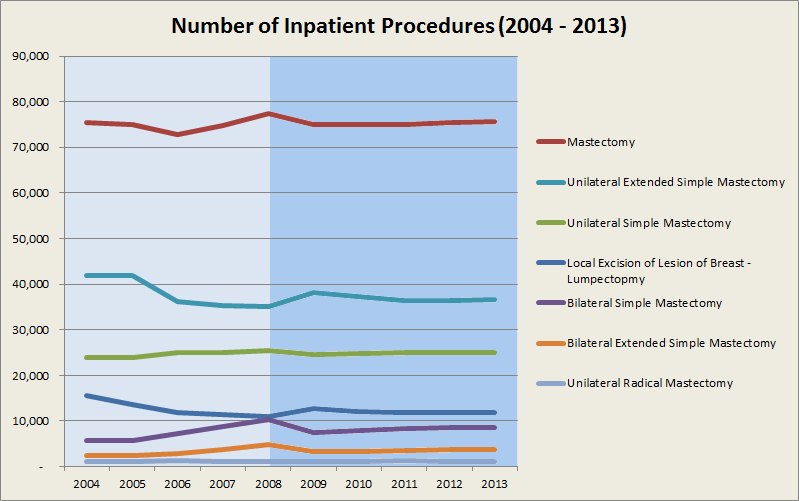
The following graph forecasts the number of procedures in mastectomy and lumpectomy for years 2009 to 2013. Please note that this is only a sample forecast and the actual forecast may differ.
Methodology
- Data to be fitted to linear and polynomial models
- Auto-regressive, integrated and moving average models and combinations of the same to be considered
- Model giving best results to be considered
- Adjustments to be made to model based on qualitative factors
Opinion Analysis
BreastCancer.org
- Alexa Rank (US) - 15,855
- Category - Health > Conditions and Diseases > Cancer > Breast
- Category Rank - 1
The websites contains a section devoted to mastectomy vs. lumpectomy. Experts from the section are as follows:
Under certain circumstances, people with breast cancer have the opportunity to choose between total removal of a breast (mastectomy) and breast-conserving surgery (lumpectomy) followed by radiation.
Lumpectomy followed by radiation is likely to be equally as effective as mastectomy for people with only one site of cancer in the breast and a tumor under 4 centimeters. Clear margins are also a requirement (no cancer cells in the tissue surrounding the tumor).
Lumpectomy: Advantages and disadvantages
The main advantage of lumpectomy is that it can preserve much of the appearance and sensation of your breast. It is a less invasive surgery, so your recovery time is shorter and easier than with mastectomy.
Lumpectomy has a few potential disadvantages:
- You are likely to have 5 to 7 weeks of radiation therapy, 5 days per week, after lumpectomy surgery to make sure the cancer is gone.
- Radiation therapy may affect the timing of reconstruction and possibly your reconstruction options after surgery. Radiation therapy also may affect your options for later surgery to lift or balance your breasts.
- There is a somewhat higher risk of developing a local recurrence of the cancer after lumpectomy than after mastectomy. However, local recurrence can be treated successfully with mastectomy.
- The breast cannot safely tolerate additional radiation if there is a recurrence in the same breast after lumpectomy. This is true for either a recurrence of the same cancer, or for a new cancer. If you have a second cancer in the same breast, your doctor will usually recommend that you have a mastectomy.
Mastectomy: Advantages and disadvantages
For some women, removing the entire breast provides greater peace of mind ("just get the whole thing out of there!"). Radiation therapy may still be needed, depending on the results of the pathology.
Mastectomy has some possible disadvantages:
- Mastectomy takes longer and is more extensive than lumpectomy, with more post-surgery side effects and a longer recuperation time.
- Mastectomy means a permanent loss of your breast.
- You are likely to have additional surgeries to reconstruct your breast after mastectomy.
Susan G. Komen for the Cure
- Alexa Rank (US) - 19,383
- Category - Health > Conditions and Diseases > Cancer > Breast
- Category Rank - 2
The website contains research tables indicating overall survival rates in mastectomy versus lumpectomy plus radiation in early breast cancer. The following table shows the research summary:
| Study | Study Population | Stage of Breast Cancer | Follow-up | Overall Survival | |
| (number of participants) | (years) | Mastectomy | Lumpectomy & Radiation | ||
| Randomized clinical trials | |||||
| NSABP B-06 | 1,851 | Stage I-II | 21 | 47% | 46% |
| EORTC | 868 | Stage I-II | 13 | 60% | 55% |
| Danish Breast Cancer Cooperative Group | 731 | Stage I-III | 20 | 58% | 51% |
| Milan | 701 | Stage I | 20 | 58% | 59% |
| National Cancer Institute | 237 | Stage I-II | 26 | 44% | 38% |
| Arriagada | 179 | Stage I | 22 | 52% | 60% |
| Pooled and meta-analyses | |||||
| EBCTCG | 4,891 | Stage I-II | 10 | 71% | 71% |
| van der Hage et al. | 3,648 | Stage I-II/III | 11 | 68% | 72% |
It is mentioned that the difference in survival rated is not statistically significant and hence there is no difference in overall survival between women treated with either method.
Key Gatekeeper Analysis
Sample (Orthopedic Surgery)
The pathway for orthopedic surgery involves patient's entry to the medical system and a passage via 'medical gatekeeper' (general practitioner or referring physician) to an orthopedic surgeon. The three important decisions that lead to a surgery are as follows:
- Patient's decision to seek help from the medical profession.
- General Practitioner (gatekeeper) decision to refer the patient to an orthopedic surgeon. (American Academy of Orthopaedic Surgeons)
- Orthopedic Surgeon decision to carry out a surgery on the patient (Oxford Journals)
It is observed in a study that the gatekeepers (general practitioner or referring physician) think that patients need to be severely affected to warrant a surgery than do the orthopedic surgeons. Therefore in many cases the referring physicians might be holding back the patients. (NCBI PubMed Journals)
Treatment Pathway
Treatment pathway is as follows:
- If the patient faces acute pain, he self-refers himself to A&E (Accident & Emergency)
- From the A&E, he is sent to an orthopedic surgeon along with his history, X-ray, MRI and blood tests
- The pre-op nurse undertakes investigation and the orthopedic surgeon undertakes surgery
- The surgery is followed by physiotherapy and the process ends
- If the pain is not acute, the patient presents himself at a general practitioner
- The general practitioner undertakes examination, sends for X-Ray
- If results are positive, the general practitioner sends a referral letter to an orthopedic surgeon and the same process is followed as in case of self-referral
- The doctor checks for anterior knee pain, BMI
- The patient is advises pharmacological and non-pharmacological therapy
- If the pain ends, the treatment is successful and the process ends
- Else, the patient is referred to an orthopedic surgeon
- The general practitioner undertakes examination, sends for X-Ray
Reimbursement Analysis
The following table shows the average medicare reimbursements for sentinel node biopsy at time of lumpectomy procedure. The medicare billing rate is for a hospital outpatient department and covers the following:
- Breast Center (Hospital Owned)
- Imaging Center (Hospital Owned)
- Radiology Department (Hospital)
- Department (Hospital Outpatient)
| Description | Facility Billing | Physician Billing |
| Injection of Dye | $180.76 | $38.97 |
| Lymphatics and Lymph Node Imaging | $258.45 | $60.62 |
| Mastectomy, Partial | $1,669.41 | $597.92 |
| Biopsy or Excision of Lymph Node(s); Open Superficial | $1,659.17 | $237.44 |
| Biopsy or Excision of Lymph Node(s); Open, Deep Axillary Node(s) | $1,659.17 | $403.06 |
Clinical Trials Analysis
| NCT Number | NCT00960154 |
| Study Sponsor | Peak Surgical, Inc. |
| Official Title | A Prospective, Randomized, Controlled Study to Evaluate Use of the PEAK PlasmaBladeTM 4.0 in Breast Lumpectomy. |
| Detailed Description | Lumpectomy is a surgical procedure performed to remove a localized mass of breast tissue that is suspicious for malignancy. The purpose of lumpectomy is to minimize the amount of tissue removed from the breast to retain normal breast architecture while simultaneously removing all of the suspected cancerous tissue. Typically, a scalpel is used for the skin incision and a traditional electrosurgical device is used to cut away any cancerous tissue. |
| The PEAK PlasmaBlade™ uses pulsed radiofrequency (RF) energy and a highly-insulated handpiece design to enable precision cutting and coagulation at the point of application. The PlasmaBlade has received FDA clearance for use in plastic, general, and ENT surgery, and has demonstrated a significantly reduced thermal injury profile in incised tissue compared to traditional electrosurgical devices. It is hypothesized that this benefit may improve the pathological analysis of excised breast lumps. | |
| Intervention | Device: PEAK PlasmaBlade - |
| The entirety of the lumpectomy will be performed with the PEAK PlasmaBlade including the skin incision. | |
| Procedure: Traditional Electrosurgery with scalpel - | |
| The skin incision will be performed using a standard scalpel; the subcutaneous dissection will be performed with traditional electrosurgery using the Cut and Coagulation modes. | |
| Start Date | July 2009 |
| Primary Completion Date | November 2011 |
Peak Surgical, Inc.
PEAK Surgical, Inc. is a medical device company that has developed the PEAK PlasmaBlade, a tissue dissection device based on a proprietary technology that represents an important advance in radiofrequency surgical technologies. The PlasmaBlades are a family of disposable cutting devices that offer the exacting control of a scalpel and the bleeding control of traditional electrosurgery without extensive collateral damage. These surgical devices come together with the PULSAR Generator, which supplies pulsed plasma radiofrequency energy to the PlasmaBlades, to form the PEAK Surgery System.
Medtronic acquired Peak Surgical in August 2011. The total value of the acquisition was $120 million.